Benign Paroxysmal Positional Vertigo (BPPV) can also be referred to as vestibular vertigo or just vertigo for short. It can affect daily activities when symptoms are provoked with head movement.
When first experienced, people commonly wake up and roll out of bed but then feel too sick to go to work. Symptoms often decrease when sitting and their coffee or tea. But when they bend over to tie their shoes, their world is likely to start spinning again.
Benign Paroxysmal Positional Vertigo (BPPV) leads 86% of affected individuals to seek medical consultation and take sick leavem, due to their inability to complete daily activities without severe symptoms. Of that 86%, only 8% receive effective treatment.1.
For effective treatment of BPPV and vertigo, talk to a CityPT clinician that specialized in vestibular care (treatment of dizziness).
Table of Contents
- Understanding BPPV
- Symptoms of BPPV
- Causes Associated with BPPV
- Diagnosing BPPV
- What to Expect from Physical Therapy
- Is It Time to Seek Treatment?
Understanding BPPV
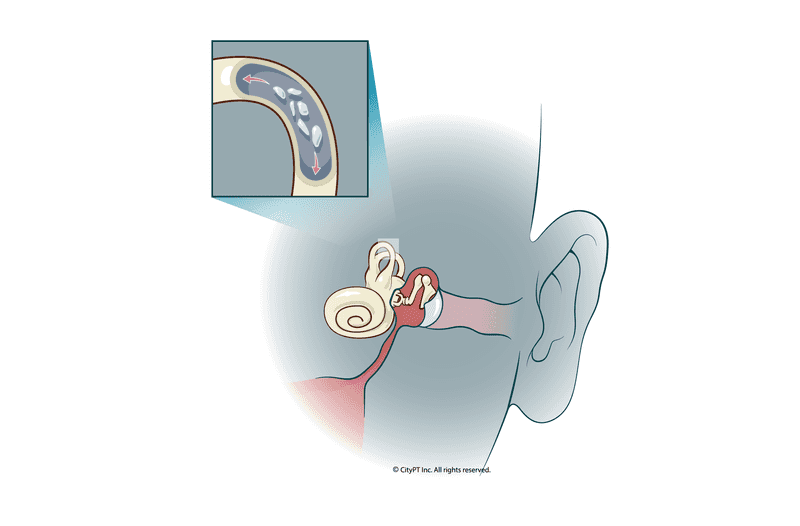
BPPV is an inner ear disorder where movement of the head can result in a sensation of movement that causes dizziness and nausea.
The inner ear, also known as the vestibular system, is how the head interprets movement. One part of the vestibular system identifies rotational movement (semicircular canals), and the other identifies acceleration movement (vestibule).
BPPV occurs when these two systems mix and a crystal (otolith) from the vestibule is circulating around the semicircular canal — causing the brain to interpret extra motion and eliciting sensations of vertigo.
To simplify BPPV we will define each of its components.
- Benign: Not harmful in effect
- Paroxysmal: A fit, attack or sudden increase of recurrence of symptoms
- Positional: Relating to/determined by position
- Vertigo: A sudden spinning sensation of yourself or your environment
Symptoms of BPPV
Let's review the most common symptoms associated with benign paroxysmal positional vertigo:
- Sensation of vertigo (room spinning) that increases with head movement
- Onset often occurs upon waking and rolling over in bed
- Sudden onset of vertigo: may or may not have a direct cause
- Eyes can have nystagmus (rapid uncontrolled eye movement) with head movements
- Symptom of oscillopsia: seeing an illusion of the environment moving sporadically (your environment is rocking like you are on a boat in rough water but you are actually standing on solid land)
- Inability to complete routine tasks because when you move your head your symptoms increase
- Extra input to your brain making it hard to concentrate and focus
Causes Associated with BPPV
The most common cause of BPPV is not well known (idiopathic)2 and often occurs spontaneously in 50 to 70 year age group.3 Head trauma is most common for adolescents and can account for up to 10% of BPPV cases across age groups 1.
Note: If you experience head trauma please seek medical care immediately.
Numerous other factors associated with BPPV include:
- Being older than 50 due to structural changes to the vestibular system anatomy
- Females more likely than males
- Migraines
- Diabetes
- Osteoporosis
- Intubation (hospitalization with tubes needed for breathing)
- Infection
- Allergies
- Menopause
- Chronic Obstructive Pulmonary Disease (COPD)
Diagnosing BPPV
Your physical therapist will discuss your medical history, how the dizziness started and what provokes it. They will then discuss how this is impacting your lifestyle and develop a treatment program to return you to function. They will also help identify if further medical consultation is needed and by which type of provider.
Diagnostic criteria for BPPV includes all of the following:1
- Sensation of vertigo is recurrent
- The sensation lasts less than 1 min
- Symptoms are provoked by head movements (laying down, rolling over, reclining your head, bending forward, standing from laying down)
- Symptoms not attributed to other conditions that can cause dizziness
During the initial exam, you can expect:
- An in-depth review of medical history, symptoms, and activity levels
- An assessment of risk factors for severe causes of dizziness
- A physical examination of neck structures and range of motion
- Eye tracking
- Head movements specific to the vestibular system
- Posture and gait analysis
What to Expect from Physical Therapy
If you are diagnosed with BPPV, your physical therapist will complete position specific maneuvers for the vestibular system to help resolve symptoms.
As your dizziness improves your PT will progress your vestibular rehab to include habituation exercises. These exercises are meant to increase your symptoms but not to push you far enough that you are too dizzy to complete your day. You can think of this as re-calibrating your nervous system to return you to bending, rolling over, looking up to the top shelf without experiencing vertigo.
Finally, they can also address any fall concerns from dizziness and help you with a home exercise program to optimize your outcomes.
Is It Time to Seek Treatment?
There are many videos out there for treatment of vertigo (BPPV) but if completed inaccurately they can actually make your condition worse and increase the length and severity of your symptoms. Your risk of falls and inadvertently limit the activities (due to activity avoidance).
According to a study completed in 2000, for North Americans "the cost of BPPV was calculated at more than $2000 per individual; most of these expenses were for unnecessary diagnostic measures and ineffective therapy."4
Our CityPT physical therapists thoroughly assess and treat BPPV effectively from the start. When treated correctly you will often be back to your non-dizzy self within five sessions or less.
Book an appointment to get started.
This guide is intended for informational purposes only. We are not providing legal or medical advice and this guide does not create a provider-patient relationship. Do not rely upon this guide (or any guide) for medical information. Always seek the help of a qualified medical professional who has assessed you and understands your condition.
References
Footnotes
-
Von Brevern, M., Radtke, A., Lezius, F., Feldmann, M., Ziese, T., Lempert, T., & Neuhauser, H. (2007). Epidemiology of benign paroxysmal positional vertigo: a population based study. Journal of Neurology, Neurosurgery & Psychiatry, 78(7), 710–715. https://doi.org/10.1136/JNNP.2006.100420 ↩ ↩2 ↩3
-
Oas, J. G. (2001). Benign paroxysmal positional vertigo a clinician’s perspective. Annals of the New York Academy of Sciences, 942(1), 201–209. https://doi.org/10.1111/j.1749-6632.2001.tb03746.x ↩
-
Hornibrook, J. (2011). Benign Paroxysmal Positional Vertigo (BPPV): History, Pathophysiology, Office Treatment and Future Directions. International Journal of Otolaryngology, 2011, 1–13. https://doi.org/10.1155/2011/835671 ↩
-
Li JC, Li CJ, Epley J, Weinberg L. Cost-effective management of benign positional vertigo using canalith repositioning. Otolaryngology–Head and Neck Surgery. 2000;122(3):334-339. doi:10.1067/mhn.2000.100752 ↩